An Innovative Early Solution for Increased Nuchal Translucency (NT)

NT: small space - big implications.
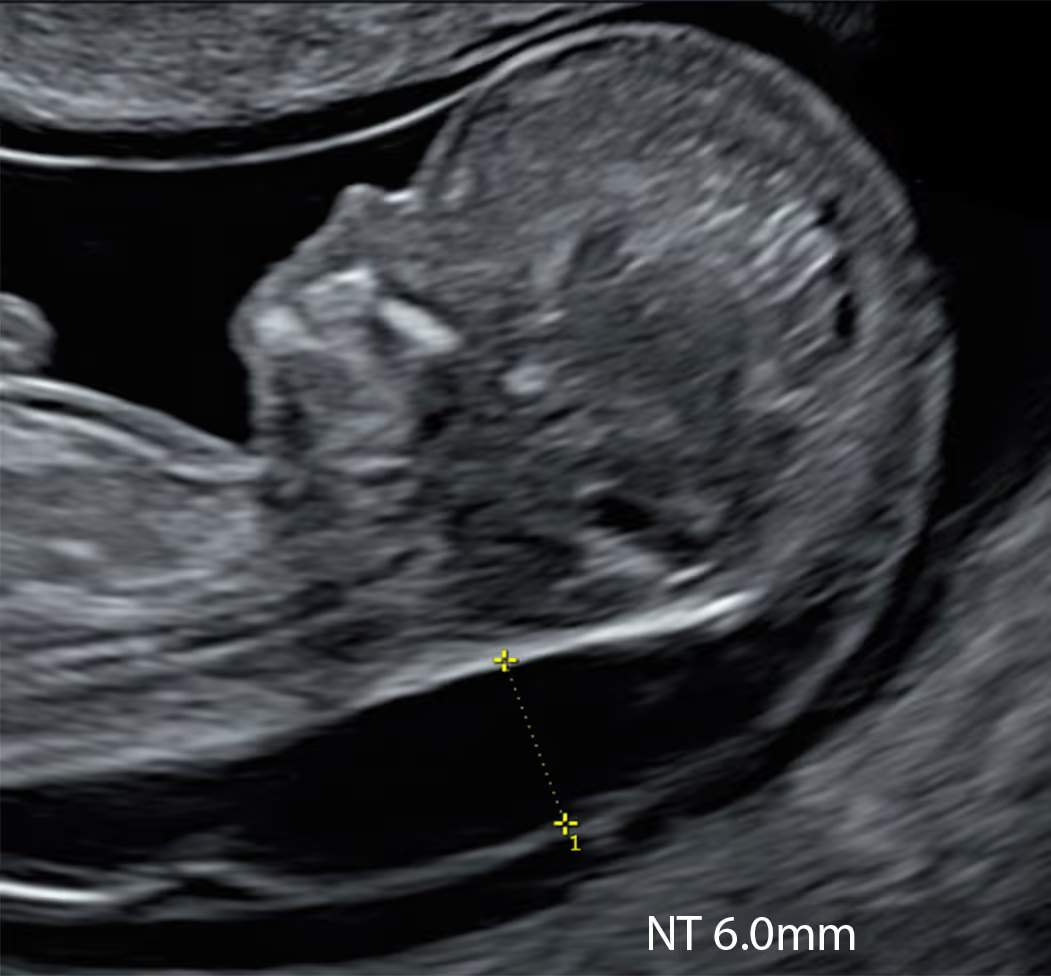
Nuchal translucency (NT) is the small fluid-filled space at the back of the baby’s neck seen on early ultrasound. A larger-than-expected NT raises the chance of chromosomal, genetic and structural conditions. Congenital heart defects prompts targeted scanning and appropriate testing.
At the standard 11–14-week scan, increased nuchal translucency (NT) is most commonly defined as ≥ 3.5 mm. At 10 weeks (CRL < 45 mm), an NT of ≥ 2.5 mm is typically used as the cut-off
Your clear guide to increased nuchal translucency (NT); what it means and what to do. Evidence-based, accessible, UK-focused, and regularly updated protocol for both parents and clinicians.
SMART NT
Earlier, smarter screening at 10 weeks - expert ultrasound plus KNOVA NIPT
A 10-week NT measurement is more sensitive and offers several benefits over the standard 11–14 week approach.
Basic NIPT is insufficient for increased NT, use an advanced assay that also covers monogenic disorders and key microdeletions.
Routine CVS or amniocentesis are non-diagnostic for monogenic conditions in high NT. Consider exome or whole-genome sequencing.
While increased NT may resolve in some cases, it is frequently associated with a broad range of serious babie's health conditions.
Increased NT is not just linked to Down syndrome. It can be associated with many other conditions, which together are more common and often more serious. The SMART NT protocol is design to screen for the majority of them.
We have developed a robust SMART NT protocol that combines the earliest possible diagnosis of abnormal NT, at 10 weeks, with advanced non-invasive genetic testing and high-resolution ultrasound – providing early diagnosis and early reassurance.
40% of fetuses with early increased NT are affected by major health issues

Testing for Multiple Chromosomal and Genetic Conditions That Could Affect Your Baby

Expert Scan at around 12-13 weeks is essential to exclude severe physical anomalies

At 10 weeks (CRL under 45 mm), an NT of 2.5 mm or more is the most commonly used cut-off to define an abnormal increase.
At 10 weeks, abnormally increased NT (>2.5 mm) is uncommon, but when present it is a clinically significant finding.
An increased NT at 10 weeks is often a stronger sign of problems than the same finding later in pregnancy.
Early increased NT resolves quickly in half of the cases, but even then about 20% of babies may still have underlying problems.
Chat with our Genetic Counsellor, receive your at-home DNA kit with a quick cheek swab, send it back, and get your results in under 4 weeks.
NT scan and NIPT at 10 weeks, then full results by week 12
1
If increased NT is found, you can have the SMART Test straight away
2
Receive genetic results in 2 weeks
3
Top-to-toe expert fetal examination
Disclaimer! These reflections are my own and arise from practice rather than committee. They do not represent the positions of the FMF, UCLH, NHS, RCOG, ISUOG, or any other organisation. As with any clinician, I may make mistakes or misjudgements. But I believe that coupling a careful 10 Week Scan with modern NIPT, and escalating to targeted diagnostics when indicated, offers families the balance we seek: early clarity without haste, and precision without noise.

Midline Section: Full CRL view showing head and trunk in mid-sagittal section. The fetus may be face-up or back-up, as long as all mid-sagittal criteria are met.
Visualise: forehead and echogenic nasal tip, brainstem with typical “Z” shape, 4th ventricle and nuchal region
Skin line must be clearly seen, either separated from or merged with amnion. Spine must be straight.
Magnification: The fetal body should fill >60% of the screen.
Calliper Placement: Callipers should be placed on the inner borders of the nuchal translucency. Measurement must be perpendicular to the skin surface (crossbar orientation).
NT scan and NIPT at 10 weeks; full results by 12 weeks
Yes. SMART NT is not just a catchy name, it describes a structured and modern way of managing pregnancies with increased NT. SMART NT refers to an advanced protocol for babies with raised nuchal translucency, based on a special version of the SMART Test® pathway.
SMART Test® (Structural, Chromosomal and Monogenic Anomalies Recognition Two-step Test®) was developed by Dr Fred Ushakov at the London Pregnancy Clinic in the 2020s. It combines a highly detailed early anatomical scan of the fetus with the most advanced forms of NIPT (non-invasive prenatal testing), usually starting from around 10 weeks of pregnancy.
The SMART NT protocol was created to improve and modernise the management of fetuses with increased NT by detecting the problem earlier (10 weeks) and using the best available ultrasound and genetic technologies to screen as thoroughly as possible for structural anomalies, chromosomal conditions, microdeletions and monogenic (single-gene) syndromes.
SMART NT itself is a screening pathway and is completely safe for the baby, as it relies on ultrasound and blood tests only. However, if NIPT or ultrasound findings raise concern, an invasive diagnostic test such as CVS or amniocentesis may still be needed to confirm the result.
The SMART NT website has been created to explain, in clear language, what an increased nuchal translucency (NT) means and how pregnancies with raised NT can be managed using the most up-to-date ultrasound and genetic tests. NT is one of the best-known terms in fetal medicine and obstetric ultrasound, yet there is surprisingly no single, truly evidence-based resource that clearly describes NT and the wide range of conditions associated with it. This site is our attempt to fill that gap.
The website is, first of all, an information resource for patients and their families – to help them understand NT, modern screening options and the questions they may wish to ask their own healthcare providers. It is not a substitute for personal medical care, diagnosis or counselling.
At the same time, it is also intended as a reference point for professionals who are involved in the care of pregnancies with increased NT, highlighting contemporary pathways that combine high-resolution ultrasound with advanced genomic testing.
Finally, the site aims to support the development of a SMART NT network around the world, promoting education, collaboration and the sharing of best practice in this rapidly evolving field.
SMART NT brings together two powerful tools – high-resolution early ultrasound and advanced NIPT – in a planned way, so that structural and genetic problems linked to increased NT can be looked for much earlier and in more detail than with standard pathways. Instead of waiting until the traditional 20-week anomaly scan, SMART NT focuses on expert scans at around 10 and 12–13 weeks, with particular attention to the baby’s heart, brain, face, abdomen and skeleton. This allows many serious anomalies that are often associated with raised NT to be suspected or diagnosed several weeks earlier.
At the same time, SMART NT uses extended NIPT panels that do more than just screen for Down, Edwards and Patau syndromes. These tests can also look for selected monogenic (single-gene) syndromes that are known to be linked with increased NT – conditions that standard invasive testing, limited to karyotype or microarray, may completely miss unless exome or whole-genome sequencing is specifically requested.
By combining what we can see on very detailed early scans with what we can detect in the baby’s DNA in your blood, SMART NT provides a much broader picture of your baby’s health, earlier in pregnancy and without any risk of miscarriage. If a concern is found, there is still the option to confirm it with diagnostic tests such as CVS or amniocentesis; if everything looks reassuring, it can give a much stronger level of early reassurance than NT measurement or basic NIPT alone.
Understandably, SMART NT is a screening pathway and cannot exclude all conditions associated with increased NT. Even with very detailed scans and advanced NIPT, some problems may still only become apparent later in pregnancy or after birth.
Even the most advanced genomic diagnostic tests based on invasive sampling (CVS or amniocentesis), including whole-genome sequencing (WGS), cannot detect all conditions associated with increased NT.
SMART NT is a dedicated pathway for pregnancies with increased nuchal translucency, not just a single scan.
A standard NT scan usually means one ultrasound at 11–14 weeks to measure the fluid at the back of the baby’s neck and, in some units, to do a basic structural check and calculate the combined screening result.
In contrast, SMART NT starts earlier (10 weeks) and combines a highly detailed anatomical scan with the most advanced forms of NIPT (non-invasive prenatal testing) in a planned, stepwise way. The aim is to pick up increased NT sooner, use high-resolution ultrasound to look carefully for structural anomalies (especially heart and brain problems), and pair this with genomic tests that can screen not only for the common trisomies but also for microdeletions and many single-gene syndromes.
SMART NT is therefore a modern, comprehensive screening protocol designed specifically for the “increased NT” scenario, whereas a standard NT scan is typically a one-off measurement used mainly to calculate combined screening.
SMART NT is built around the early pregnancy window, starting from 10+0 weeks. By 10 weeks of pregnancy (around 8 weeks after conception), virtually all major organs have begun to form in the fetus. This point marks the end of the embryonic period and the beginning of the fetal stage. Coincidentally, 10 weeks is also the stage at which NIPT performance becomes robust.
We recommend a first visit at 10 weeks, where you have an advanced high-resolution scan with a detailed NT assessment. If the NT is raised (from the 95th centile for CRL) or clearly abnormal (2.5 mm or more at 10 weeks), blood is taken at the same appointment for advanced NIPT. This means that both the ultrasound assessment and the genetic screening are initiated as early as possible.
A second visit is usually arranged once the NIPT results are back, typically around 12–13 weeks. At this stage, a more detailed early anomaly scan is performed, with particular attention to the baby’s heart and other organs, and the findings from both the scan and the NIPT are reviewed together. If the NIPT result is high chance, and/or the fetus has persistent increased NT or structural anomalies, the options for invasive diagnostic testing (CVS or amniocentesis) are then discussed.
SMART NT is a clinical care pathway, not a research trial. It has been developed from many years of experience in fetal medicine, drawing on robust evidence from published studies together with modern advances in ultrasound and genomic testing.
Parents are not “recruited”, randomised or exposed to experimental procedures. Instead, SMART NT organises already validated high-resolution ultrasound and modern genomic tests into a structured, early pathway for pregnancies with increased NT.
Fetal anatomical scans at 10–14 weeks have been validated in multiple large studies around the world, including hundreds of thousands of fetuses. The ability to detect heart anomalies in the first trimester has been confirmed by a major meta-analysis of more than 300,000 fetuses.
Likewise, genomic technology for monogenic NIPT has been validated in multiple research studies, and in some countries (including NHS England) this technology is even used in a diagnostic context under the term NIPD (non-invasive prenatal diagnosis), rather than purely as screening NIPT.
So, while data from SMART NT is strictly audited, for you as a parent it is offered as up-to-date, evidence-based routine clinical care – not as participation in an experimental study.
For medical professionals who want to learn more about the SMART NT approach, access training, and join our clinical network.