
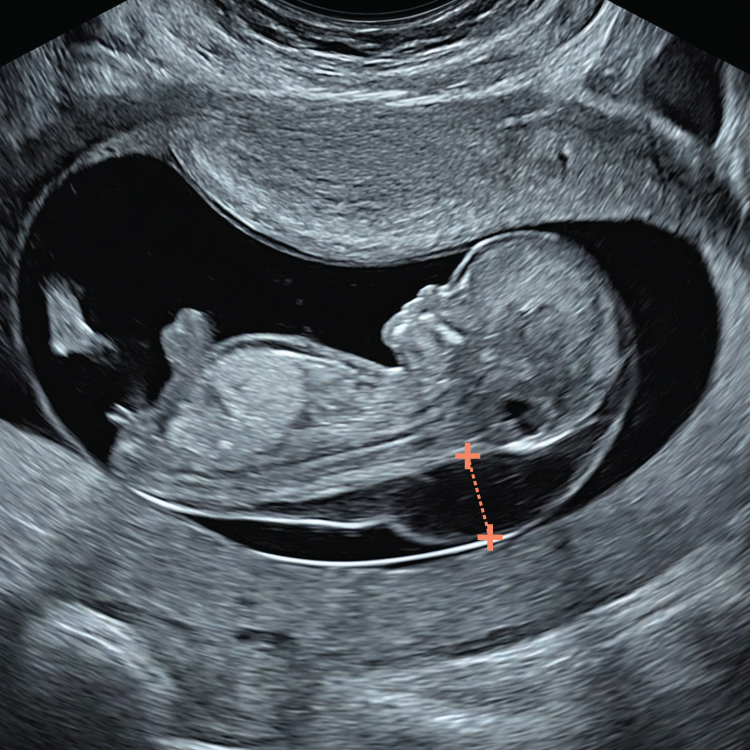
Ten weeks marks a major milestone in human development, the transition from an embryo to a recognisably human fetus.
iNT denotes increased NT at 10 weeks (CRL <45 mm) and is strongly linked to adverse outcomes - assess without delay

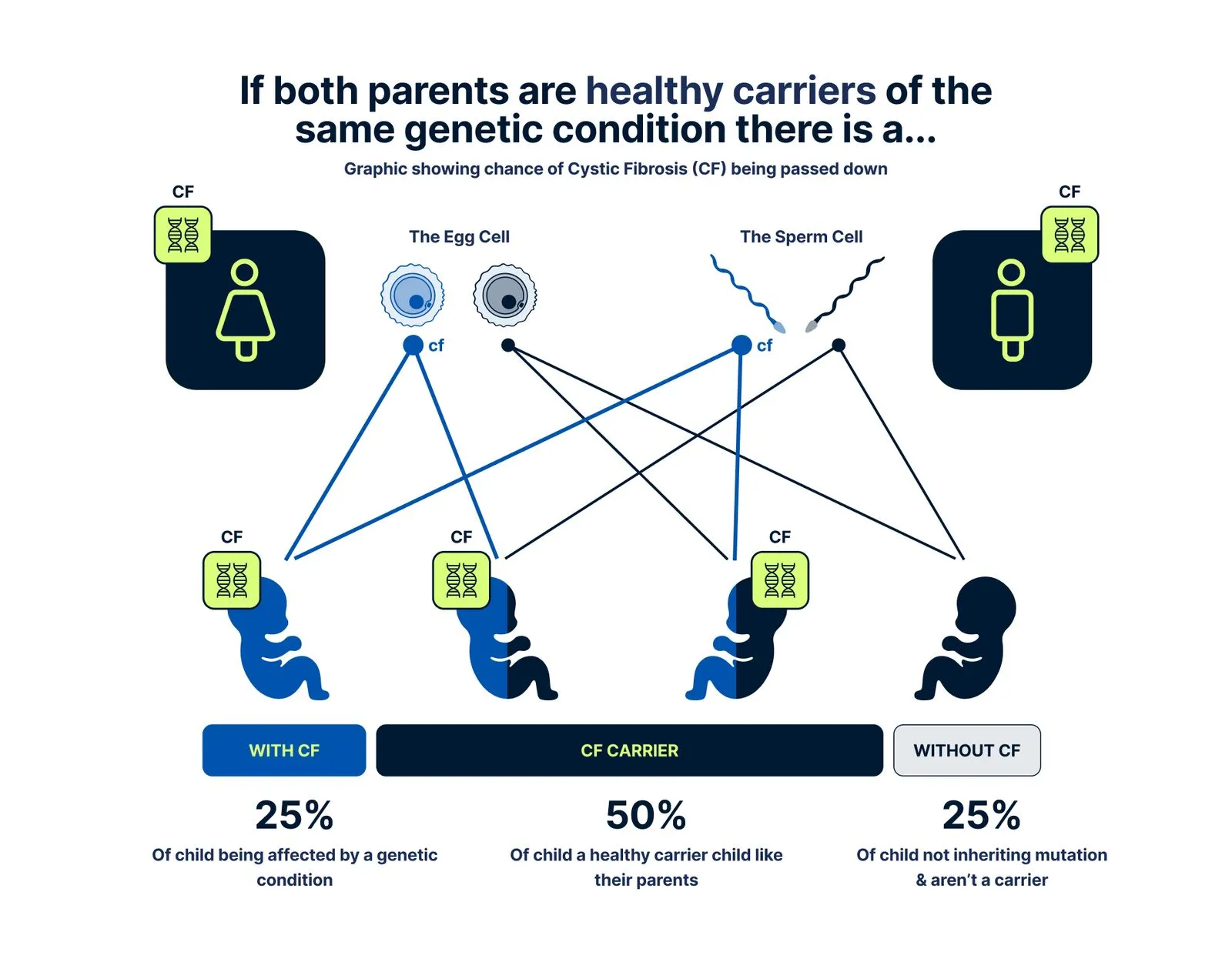
Chat with our Genetic Counsellor, receive your at-home DNA kit with a quick cheek swab, send it back, and get your results in under 4 weeks.


.avif)


In 1990, increased NT at 10 weeks was linked to fetal problems, but the finding was set aside at the time because no effective intervention was available. With today’s advances in genomic NIPT and high-resolution ultrasound, this limitation has been overcome. As a result, we developed the SMART NT protocol - a safe and effective solution for managing early increased NT. It delivers rapid risk stratification, and a clear plan for confirmatory diagnostic test (CVS) if needed.

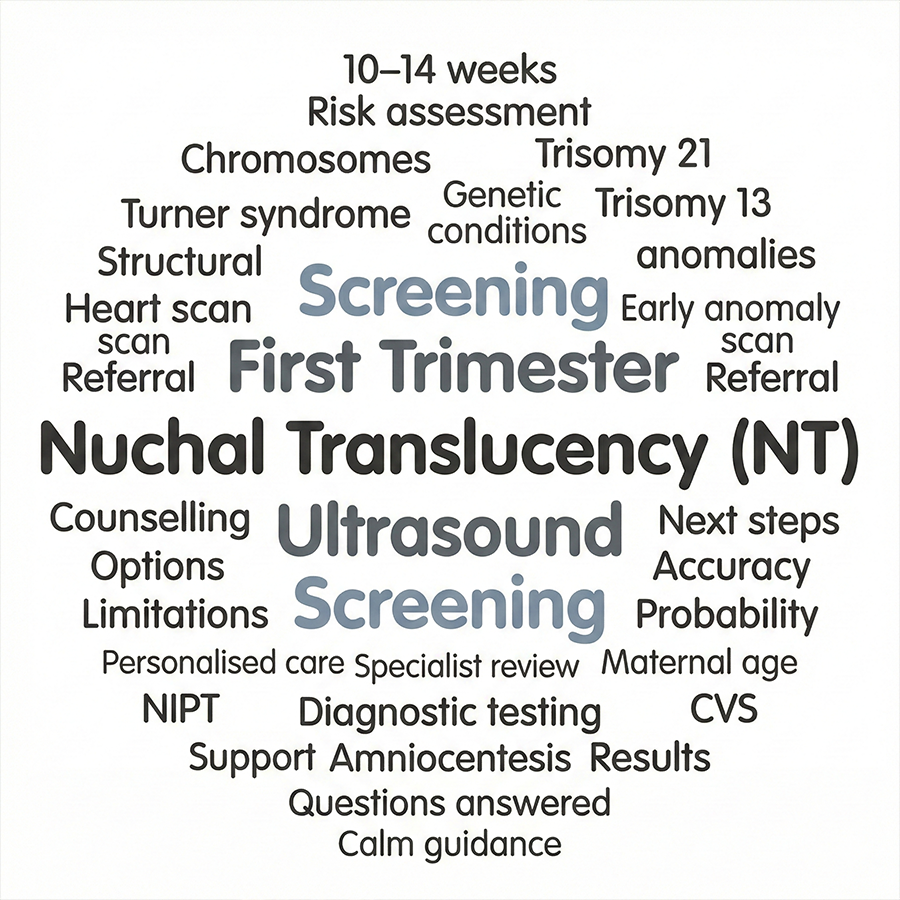
There are three different periods when nuchal thickness can be measured
At 10 weeks, NT can be measured accurately and may be a more sensitive early sign of possible problems, allowing prompt reassurance or testing.
This is the traditional time for NT assessment as part of the Combined Screening Test (CST). In the UK and many other countries, most babies have their NT measured during this stage of pregnancy.
After 14 weeks, the fluid behind the baby’s neck usually disappears, making the NT measurement unreliable. Instead, a different marker called the nuchal fold (NF) can be measured at this stage.
Increased NT Cut-off day by day chart.
You simply cannot apply the classic 11–14-week NT rules to a 10-week fetus, which is why we developed specific 10-week NT criteria. At 10 weeks the fetus is smaller, has different proportions and is structurally less mature than at the standard 12-week scan.
This becomes especially important when you are trying to measure a significantly increased NT. You cannot zoom in to a strict “head–chest” view as recommended later in the first trimester, because the whole fetus will not fit the screen and excessive magnification makes the NT borders blurred and difficult to measure accurately. At 10 weeks the fetus is also missing some key landmarks used later, such as the nasal bone.
Using a CRL-type sagittal image rather than a classic NT-type view optimises workflow, reduces scanning time and fetal exposure, and frees more time to assess vital structures such as the brain and spine.
By the way, this CRL-type view was also used by Prof Nicolaides’ group when they were scanning fetuses at 10 weeks in the early 1990s.
In quite a large proportion of babies at 10 weeks, the fluid space at the back of the neck is so thin that we cannot see or measure it reliably. This is actually reassuring and we regard it as a normal NT. To our knowledge, there are no conditions associated with a very small or “absent” NT, whereas certain problems are linked with an increased NT. So if the NT is too small to measure, that is considered a good sign rather than a cause for concern.
No, we do not use the nasal bone (NB) as a screening marker at 10 weeks. At this gestation, the only ossified facial bones are the upper and lower jaws; the nasal bone is not visible in virtually all fetuses. Trying to include NB in a 10-week checklist would therefore create many “absent NB” reports, a high false-positive rate and unnecessary anxiety.
In addition, the 10 Week Scan & NIPT approach screens for Down syndrome using cfDNA rather than ultrasound or biochemical markers, which provides much better detection with far fewer false positives.
The short answer is no; although technically we can visualise the ductus venosus and record a Doppler waveform at 10 weeks.
In practice, however, we do not use DV as a screening marker at this stage. Abnormal DV (reversed a-wave or high PI) has only modest performance for chromosomal anomalies and heart defects even in the standard 11–14-week window. There is essentially no evidence base for application of DV at 10 weeks and a high risk of false positives and unnecessary anxiety.
DV assessment requires pulsed Doppler and longer insonation, which conflicts with the ALARA principle when there is no clear, proven clinical benefit at this gestation.
In the era of highly accurate NIPT for trisomies, DV at 10 weeks is essentially purposeless, adds time to the scan, and distracts from what matters most: a high-quality NT measurement and careful early anatomical and cardiac assessment.
In theory, tricuspid regurgitation can be detected with colour and pulsed Doppler at 10 weeks, but we do not use it as a screening marker at this gestation.
Even in the classic 11–14-week window, TR adds only limited value for detecting chromosomal abnormalities and heart defects, and at 10 weeks there is virtually no robust data on its performance. Because the fetal heart is very small, TR assessment at this stage is technically demanding, prone to artefact and likely to generate false positives and unnecessary worry.
It also requires prolonged use of Doppler, which is difficult to justify under the ALARA principle when there is no clear proven benefit.
In the context of modern NIPT for aneuploidy, spending time on TR at 10 weeks brings little or no advantage and is far less important than obtaining a good NT measurement and a careful overview of early cardiac and anatomical development.
Prof Kypros Nicolaides and his group in 1992. NT assessment at 10 weeks was initially very popular, but in the late 1990s practice shifted to the FMF 11–14-week window. The main reasons were the limited resolution of older scanners, which made accurate measurement difficult in some cases, and the absence of NIPT or other suitable follow-up tests at 10 weeks at that time.
In thousands of 10 Week Scans, we haven’t seen an NT under 2.5 mm later increase to ≥3.5 mm at 11–14 weeks. Most fetuses with chromosomal and genetic conditions or structural anomalies already showed iNT at the 10 Week Scan, before NIPT.
We suspect some babies with trisomy 21 may develop a rise in NT after 10 weeks, but we have not observed this in our cohort to date. Because we offer NIPT to everyone, most babies with trisomy 21 were found by NIPT rather than a late rise in NT.
There are possibly other, less common reasons why a normal NT can increase after 10 weeks. Future studies may refine this, but that is our day-to-day experience.
It is not too early to look at NT at 10 weeks, but most traditional or standard pathways are built around the 11–13+6 week “combined test” window, so many women are simply told to wait until around 12 weeks.
The traditional approach works reasonably well for population screening, but it has limitations: if NT is increased, you only find out later, you may then need further scans and tests, and everything, including NIPT and diagnostic tests, is pushed further into the pregnancy. Moreover, non-chromosomal monogenic diseases are often diagnosed very late in pregnancy or even missed.
With the SMART NT pathway at 10 weeks, we deliberately bring the detailed scan and NT measurement earlier, in a centre experienced in early fetal anatomy. This allows earlier reassurance when everything looks normal, earlier use of NIPT (including extended or monogenic options where appropriate), and earlier identification of babies who may need targeted follow-up such as heart scans and detailed anatomy scans around 12–13 weeks, or diagnostic testing.
In conclusion, starting at 10 weeks gives you more time, more information and more options, rather than waiting passively for the 12-week scan.
In our experience, the phenomenon of increased NT can already be seen from around 9 weeks, but there are no robust cut-offs or reference ranges validated for this stage, and most NIPTs are not applicable or validated before 9 weeks.
In practical terms, if the fetus appears to have an increased NT before 10 weeks, we document this and recommend a targeted re-scan at 10 weeks. From 10 weeks onwards, NT measurement is more technically reliable and reproducible, and if the NT is still outside the normal range at that point, we proceed according to the SMART NT protocol.
Not exactly. At 11–13 weeks, NT is mainly used to calculate the probability of trisomies 21, 18 and 13 as part of the Combined Screening Test, and only secondarily as a general risk marker for other fetal problems.
In the “10 Weeks Scan & NIPT” approach, we do not use NT to screen for trisomies 21, 18 and 13, because NIPT does this far better, with a detection rate above 99%. Instead, NT at 10 weeks is used primarily as a powerful early marker of overall fetal health. Cut-offs such as the 95th centile or 2.5 mm (depending on the clinic protocol) are used as a trigger to offer the SMART NT pathway, including extended NIPT and a targeted follow-up scan at 12–13 weeks.
The NT scan at 10 weeks is just as safe as any routine pregnancy ultrasound. It uses harmless sound waves, not radiation, and we follow strict safety rules (including keeping the scan as short as reasonably possible) throughout.
The main difference is that the doctor/sonographer looks more closely at the baby’s neck area and early anatomy, but this does not make the scan “stronger” or more risky. In experienced hands on modern equipment, a 10-week NT scan is a safe, gentle and very useful check on your baby’s early development.
In most standard pathways the usual response is simply to wait and repeat the scan in the 11–14 week window, which we feel is outdated in the era of high-resolution ultrasound and advanced NIPT.
If NT is increased at 10 weeks in our clinic or any other affiliated clinics, we offer the SMART NT protocol, which includes early counselling, extended NIPT (such as KNOVA) and a targeted follow-up scan at 12–13 weeks with detailed assessment of the heart and anatomy.
This approach aims to give you earlier answers and a clearer plan; more details are available on the SMART NT pages of our website.
Definition of iNT: iNT denotes increased nuchal translucency at 10 weeks (CRL <45 mm), defined as NT ≥2.5 mm. It is strongly associated with adverse outcomes and should prompt timely, expert evaluation.
From 11–14 weeks (CRL 45–84 mm), NT terminology is confusing. Inconsistent terms include “increased/raised/thickened/large/abnormal NT”, “screen-positive NT”, “high-risk NT”, “nuchal edema”, “>95th centile”, “>99th centile”, and cut-offs such as NT ≥3.0, ≥3.5, or ≥4.0 mm; “cystic hygroma” is also sometimes used interchangeably.
To avoid ambiguity, use “iNT” only at 10 weeks with the 2.5 mm cut-off; do not use iNT for later stages to avoid confusion.
This area has, surprisingly, not been properly evaluated. The traditional 11–13+6-week window was deliberately chosen. Existing data suggest that both 10-week NT and biochemical markers (especially PAPP-A) may perform better at 10 weeks than in the traditional window, but this has never been implemented clinically. The most likely reason is the introduction of NIPT in 2010s, which made further improvement of the Combined Screening Test largely obsolete and interest in developing it further has faded.
Our team of experts is here to help. We're just a message away.