Non-invasive prenatal testing (NIPT) is a maternal blood test that analyses placental cell-free DNA to screen for chromosomal and monogenic syndromes.
Because NIPT analyses cfDNA and cannot detect fetal structural anomalies, it must be combined with ultrasound, such as a 10 Week Scan, for structural assessment.
NIPT is highly accurate but not diagnostic; positives require confirmation by CVS or amniocentesis.

Chat with our Genetic Counsellor, book your at-home NIPT blood draw with a professional nurse, and get your results in under 4 weeks.

NIPT (non-invasive prenatal testing) is: a blood test that analyses placental (fetal) cell-free DNA (cfDNA) in maternal blood to screen for fetal chromosomal and selected single-gene (monogenic) conditions.
The placenta develops from the same fertilised egg as the baby and therefore largely shares the baby’s genetic make-up. Placental cells are continually shed and, as they break down, release small fragments of cfDNA into the mother’s blood.
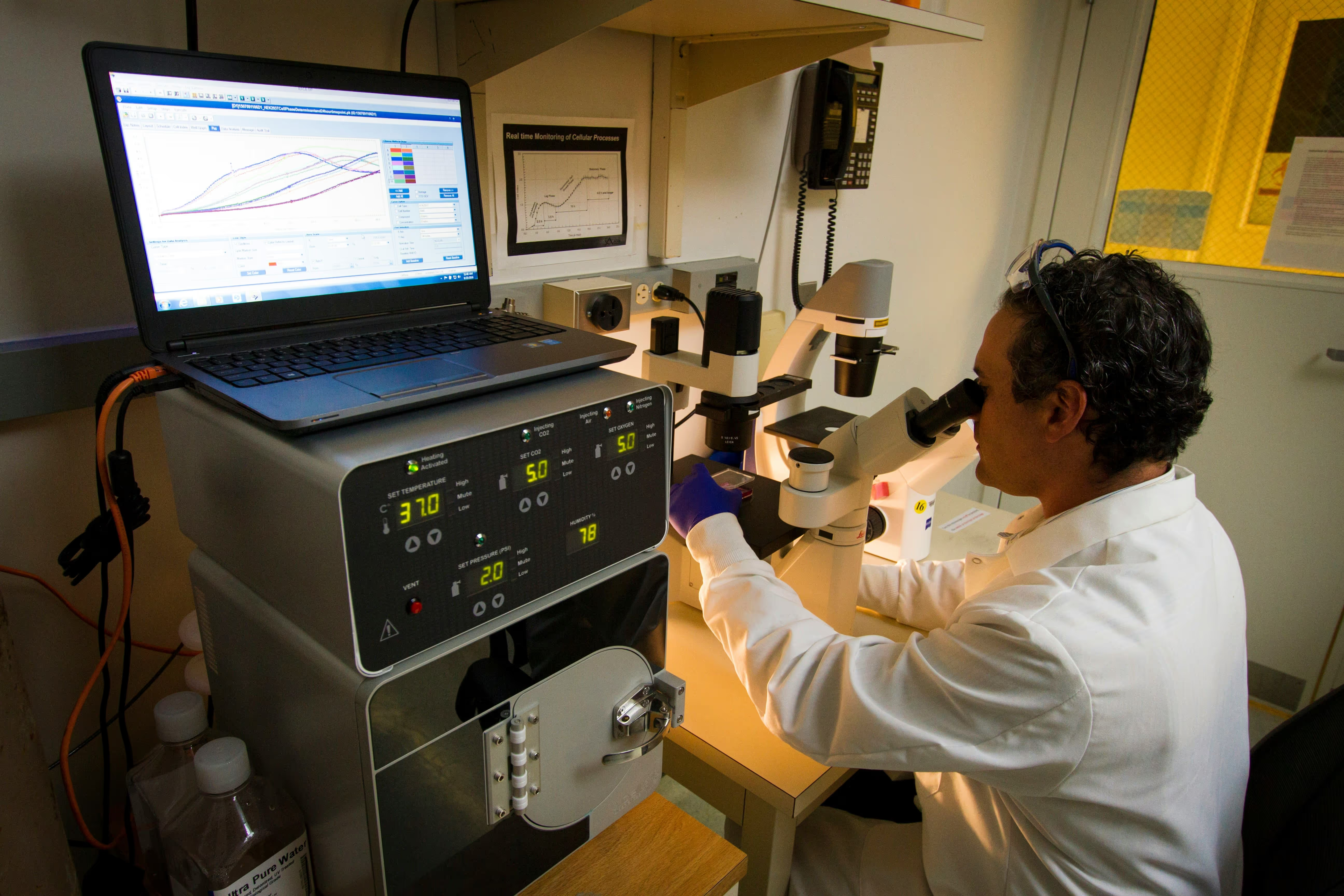
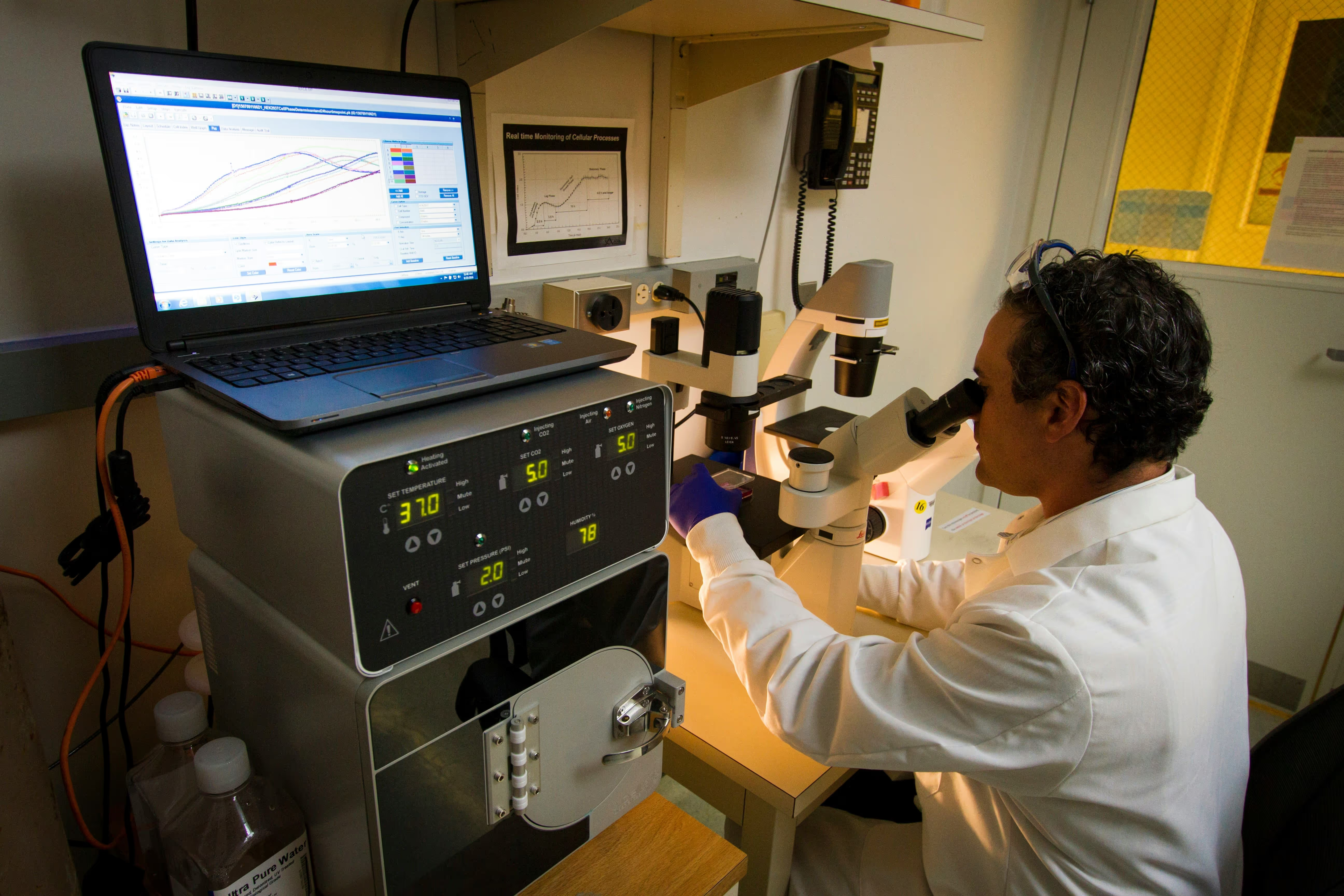
Modern genetic laboratories can distinguish placental (fetal) cfDNA from maternal DNA, analyse it, and use bioinformatic algorithms to screen for specific fetal conditions. NIPT is completely safe, as it uses just maternal blood sample, and highly accurate, but it is a screening test - not diagnostic.
While standard NIPT focuses on trisomies 21, 18 and 13, advanced cfDNA assays can also screen many high NT- associated conditions
Down syndrome, other aneuploidies, and sex chromosome anomalies
DiGeorge Syndrome and other copy-number variants (CNVs)
Most genetic syndromes are monogenic, such as Noonan syndrome




.avif)
.avif)
Learn about our carefully selected list of genes relating to your baby's health.
To view the table rotate phone 90 degrees.
Transparent. Personalised. No surprises.
NIPT gives you a safe and early look at your baby’s health – explore the conditions we can screen for during pregnancy
A highly accurate NIPT that screens for common and rare genetic conditions in your baby – including microdeletions.

Comprehensive blood tests for cancer markers, helping detect risks early with results guided by medical specialists.

Advanced NIPT available for single or twin pregnancies, egg donors and IVF. Optional panels for microdeletions and rare syndromes.

A cost-effective, high-quality NIPT that screens for common conditions and can include testing for inherited conditions.

Basic NIPT screens for the three most common chromosomal conditions: Down’s syndrome (Trisomy 21), Edwards’ syndrome (Trisomy 18), and Patau’s syndrome (Trisomy 13). Advanced NIPT includes everything in the basic test, but can also check for sex chromosome conditions, some rare genetic deletions (called microdeletions), and can tell you the biological sex of the baby if you choose to know.
At Jeen, our genetic counsellors will help you decide which version is right for you during your consultation.
We ask you to send us your scan so our medical team can confirm that you’re at least 10 weeks pregnant and that the pregnancy appears to be developing normally. This helps us ensure the test is appropriate and that the results will be accurate. It’s also important to understand that NIPT only screens for specific genetic conditions. It does not detect structural anomalies, such as heart defects or issues with organ development, which are physical rather than genetic. These types of conditions are usually picked up later in pregnancy through detailed ultrasound scans. Sending your early scan allows our doctors to check for any concerns before moving forward with the NIPT.
Yes, NIPT can usually identify the baby’s biological sex with high accuracy, but this is completely optional. If you’d like to know, just let your genetic counsellor know during your consultation — and if you’d rather not find out, we’ll make sure it’s not included in your report.
At the moment, NIPT is only offered through the NHS in certain cases — for example, if you’ve had a high-risk result from a standard screening test. At Jeen, we offer private NIPT testing with flexible options, fast results, and full clinical support, including at-home appointments and expert guidance.
Your results will usually be ready within 2–10 working days from the time your sample arrives at our partner lab. The exact turnaround time depends on which NIPT you’ve chosen and the location of the laboratory. We’ll keep you informed throughout the process and arrange a follow-up consultation to talk you through your results as soon as they’re ready.
Please note that delays can occur during public holidays in both the UK and the US. If your results indicate that follow-up testing is needed for your partner, we’ll act quickly to keep everything moving smoothly. Our priority is to get you the answers you need without unnecessary delays — so you can make confident, informed decisions for your pregnancy.
You can take the NIPT from 10 weeks into your pregnancy. Before booking your test with Jeen, we ask you to send us a recent pregnancy scan, such as a dating or viability scan, so our team of specialists can confirm you’re eligible to proceed.
Yes, NIPT is completely safe for both you and your baby. It’s a non-invasive blood test that only requires a small sample from your arm, and there is no physical contact with the baby. This means there is no risk of miscarriage or harm to the pregnancy, unlike some invasive procedures.
NIPT is over 99% accurate at detecting Down’s syndrome and also highly reliable for Edwards’ and Patau’s syndromes. It is more accurate than standard NHS screening and produces fewer false positive results, which means fewer people are sent for unnecessary follow-up testing.
Yes, at Jeen we believe it’s important that everyone taking NIPT has a chance to speak to a qualified genetic counsellor first. This session helps you understand what the test covers, what it doesn’t, and what the results might mean for you and your baby. It’s a space to ask any questions and make confident, informed choices.
If your result shows a high risk for a condition, we’ll arrange a follow-up session with one of our genetic counsellors to explain exactly what it means. You’ll be given the option to have a diagnostic test, such as amniocentesis or CVS, which can confirm the result. We’ll support you at every step, with clear information and no pressure.
No, NIPT screens for a specific set of genetic conditions, mostly involving extra or missing chromosomes. It won’t detect all birth defects or structural anomalies, such as heart defects or limb differences. That’s why it’s important to still attend all your routine scans and check-ups during pregnancy.
Our team of experts is here to help. We're just a message away.